The ECMO Circuit:
The basic operating principle behind ECMO is that a portion of the patient's blood is removed from the intravascular space, passed through a circuit which provides oxygen and removes carbon dioxide, and then returned back to the bloodstream. The main components of an ECMO circuit are the drainage and return cannulas, the centrifugal pump, the blender, the oxygenator, and the controller.
Drainage and Return Cannulas:
The drainage cannula allows blood to flow through the pump to the oxygenator. The return cannula returns blood from the oxygenator to the patient. Patients very often have a large proportion of their blood volume flowing through the ECMO circuit in order to be supported. The typical adult ECMO circuit handles anywhere between 1-6 litres per minute of blood flow, so large bore cannulas are needed to accommodate this.
The key points about the drainage and return cannulas are:
- They are typically 23-29 French (about 7.5 - 10 mm in diameter)
- The larger the cannula, the less resistance to flow it has
- The shorter the cannula, the less resistance to flow it has
- Drainage cannula are situated in large central veins, typically IVC, SVC, or the right atrium (this is discussed further in the next section)
- Depending on the configuration (see the next section), return cannula are situated either in the right atrium, or in the aorta
- The drainage cannula often have multiple orifices so they drain all along their length.
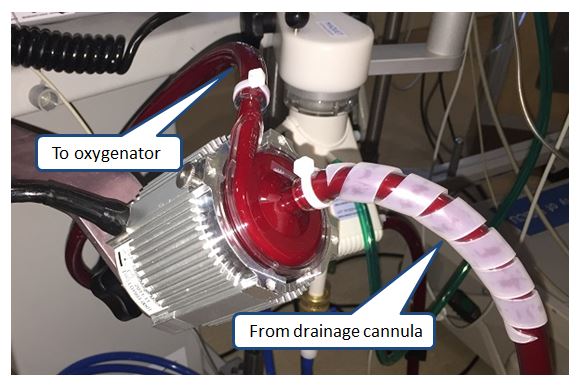
The Centrifugal Pump
Most adult ECMO circuits use a centrifugal pump to pass the blood through the circuit. A rotating configuration of blades (called an impeller) is coupled magnetically to a motor. The blades spin to create a vortex which creates a pressure differential to drive blood through the circuit.
The key points about the ECMO pump are:
- The rotation is set at a constant rate, so the rate that blood travels through the pump is continuous and not pulsatile
- The rate that blood travels through the pump is referred to as the flow of the circuit
- The pump speed is in revolutions per minute (RPM)
- Typical pump speeds are about 2000-6000 RPM
- Pump speeds higher than 4500 RPM are associated with significant hemolysis
- Flow through the pump depends on 3 things:
- Pump speed: the higher the speed, the more flow through the pump.
- The blood volume available: this can be thought of as the "preload": the more blood available to the pump, the higher the flows it can achieve.
- Downstream resistance: this can be thought of as "afterload": the more resistance the pump is facing, the less flow the pump can achieve.
- If the pump is set to 0 RPM, blood can actually flow backwards through the circuit
If the motor is functioning properly, it should never become too hot to touch. If the motor does become very hot then something is wrong and the circuit should be inspected immediately (see troubleshooting chapter for more details)
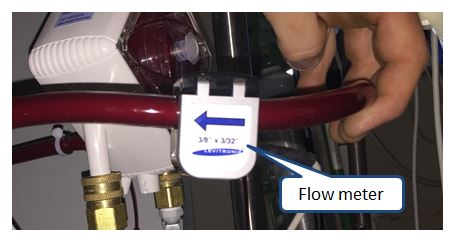
Flow Meter
- Flow through the cannulas is measured by a flowmeter which clips directly onto the cannula
- Traditionally it is placed on the arterial, or return cannula.
- The arrow on the flowmeter corresponds to the direction of blood flow.
- If the arrow is placed in the wrong direction, the flow reading will be inaccurate and the alarm will sound.
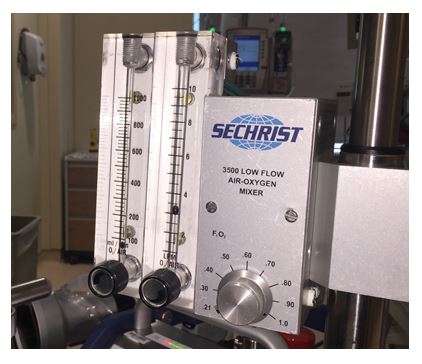
Blender
- The blender is a device which provides fresh gas to the oxygenator. The gas is a mixture of nitrogen and oxygen.
- The desired fraction of oxygen is programmed and varies from 21% (room air) to 100%.
- Typically at TGH the blender is kept at 100% oxygen unless there are specific circumstances which dictate otherwise. (see later chapters)
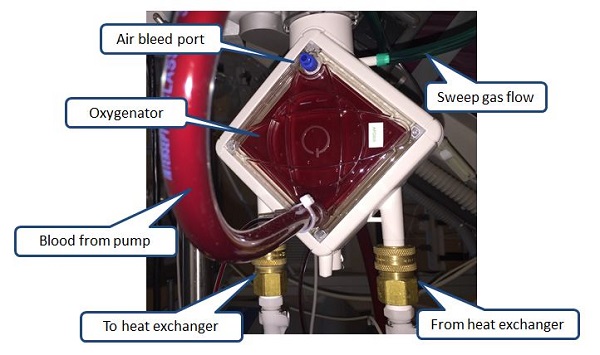
Oxygenator
The oxygenator is the most complicated component of the ECMO circuit. It is essentially a large thin membrane made of a polymer which allows gas to diffuse across it. In the oxygenator:
- The two functions are to oxygenate the patient's blood and remove carbon dioxide.
- Blood from the drainage side is pumped in on one side of the membrane, and gas from the blender is pumped into the other side.
- The rate that gas is delivered is referred to as the sweep and can be set anywhere between 0-15 L/min.
- Oxygen diffuses across the membrane the blood and carbon dioxide diffuses out.
- The blood then leaves the oxygenator and enters the return cannula where it is delivered back to the patient.
- The blood is warmed to approximately 37 degrees.
- While some ECMO circuits can actively cool patients, at TGH the circuit can only warm, not cool.
The sweep gas (green tubing) is often delivered to the oxygenator via a flowmeter attached to the wall supply of oxygen near the head of the patient’s bed. These flowmeters are often used for other purposes and it is easy to get them mixed up or to accidentally unplug the sweep gas tubing. Be careful!
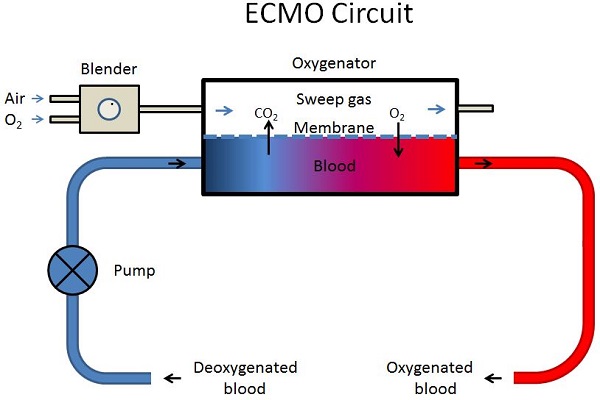
Oxygenation depends on:
- The flow, higher flows allow more blood to be oxygenated.
- The FiO2: increasing FiO2 achieves a higher partial pressure of oxygen.
- The membrane integrity: if there is something present on the membrane (e.g. blood clots) that impairs diffusion, oxygenation will decrease.
Carbon dioxide removal depends on
- The sweep: higher sweep speeds result in higher CO2 removal.
- The flow: if the flow is increased without increasing the sweep, then CO2 removal can be impeded.
- The presence of water vapour in the membrane: this can impede CO2 removal.
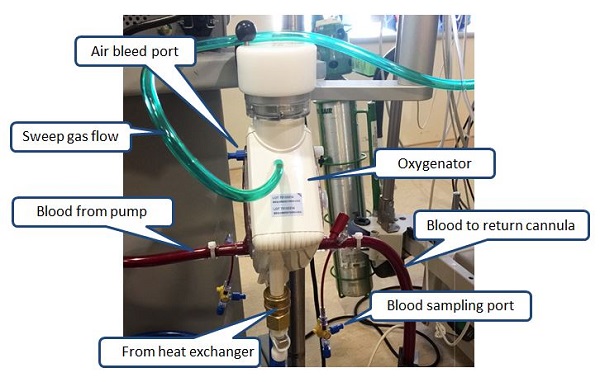
The oxygenators at TGH have two additional access points (see image):
- The port with the yellow cap on the venous drainage side is a one way valve which acts as an air vent when it is opened, but blood will NOT drain out.
- The port should never be left open to air, or there is risk of the valve crusting over with precipitated plasma.
- The port on the return side WILL allow blood to drain if it is opened, and should not be accessed at any time.
Note that oxygenation does not depend on the sweep. Of course, if the sweep is set to zero then no gas will enter the membrane and no oxygenation will occur. But in general above 1 L/min, changing the sweep across a wide range does not affect oxygenation.
NEVER SET THE SWEEP TO ZERO IN A VA ECMO PATIENT AS THIS WILL CREATE A TREMENDOUS SHUNT AND CAN LEAD TO LIFE THREATENING HYPOXEMIA
Heat exchanger
The oxygenator is connected to a heat exchanger which allows the blood to be warmed as it passed through the oxygenator.
- Blood in the ECLS circuit is exposed to the ambient temperature so it must be warmed to avoid heat loss.
- The ECLS circuit has a heat exchanger, and when it is active, it warms the blood to 37 degrees Celsius
- At TGH, the heat exchangers are not equipped with a cooling function, they can only heat blood.
- If the patient is experiencing excessively high temperatures, the heat exchanger may be turned off, and the blood will be passively cooled by the temperature of the room.

Controller
The controller allows the operator of the ECMO circuit to adjust the settings as needed. The settings that are typically adjusted are:
- The RPM: The higher the RPM, the higher the rate of blood flow through the pump.
- The sweep: More gas entering the oxygenator allows for better CO2 removal.
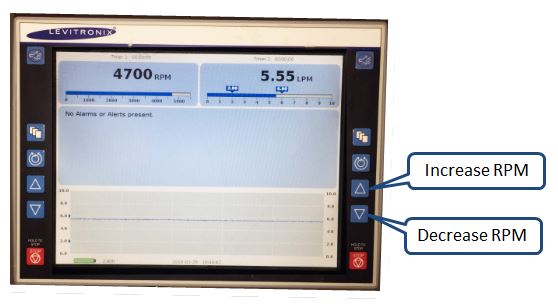
The controller has a pole-mounted graphic display that allows the adjustment of the pump RPM:
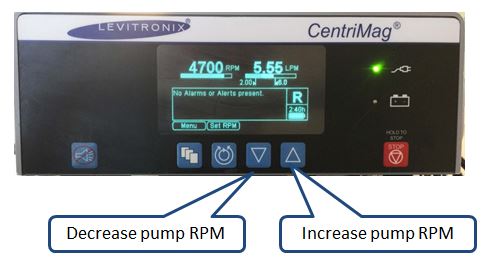
The pump RPM can also be adjusted directly on the pump controler:
Powering the ECMO circuit
- The ECMO circuits at TGH run on 120 V AC power, and have a battery pack for backup and transportation
- The power supply must be directly plugged into a red outlet located on the wall.
- It must never be plugged into a power bar.
- ECMO circuits are all equipped with a battery for backup power, but it typically lasts only a couple of hours.
- At TGH there is no manual hand crank system in the event that the ECMO machine cannot be powered.
ECMO Configurations:
There are two distinct configurations of the ECMO circuit which provide the patient with different physiologic support:
- Venovenous ECMO (or V-V ECMO)
- Venoarterial ECMO (V-A ECMO)
Nomenclature:
Before getting into specific configurations, it is important to understand how to describe ECLS configurations using a common language. The ELSO has developed a nomenclature for describing ECMO configurations. The following description is adapted from the official treaty for Nomenclature in Extracorporeal Life Support (Conrad et al, AJRCCM 2018)
- All drainage cannulas are written on the left side of the hyphen, and return cannulas on the right.
- All cannulas contributing to the primary (major) draining and return circuit flow are written in upper case letters.
- For example 'V-V ECMO' would represent venous drainage and venous return for venovenous support.
- All cannulas with minor flow for secondary drainage, unloading of specific anatomical location, or to promote distal perfusion are written in lower case letters after the major flow cannula to which side it belongs.
- For example 'V-Aa' represents venous drainage, arterial return and secondary arterial return such as for distal perfusion.
- The use of a dual lumen cannula for venovenous support would be indicated with a preceding '(dl)' abbreviation e.g. '(dl)V-V'.
- The vessel that is cannulated is described using subscripted lower-case letters. Two common examples include:
- The traditional two cannula venovenous configuration with drainage from the femoral and return to the internal jugular would be indicated as 'Vf-Vj'.
- Bifemoral cannulation for venoarterial support would be indicated as 'Vf-Af'.
Next page: ECMO Configuration: V-V ECMO
