Mechanical Ventilation: Ventilator Specifics:
Modes of Mechanical Ventilation:
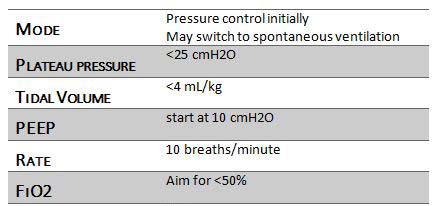
- Patients should be on pressure control ventilation for at least the first 24 hours.
- Patients can be switched to spontaneous ventilation when able, with high levels of PEEP.
- Airway pressure release ventilation is another possible spontaneous ventilation mode, but this isn't typically used at TGH.
Pressure and Volume Settings:
- "Ultra-protective" lung ventilation is recommended, keeping tidal volumes < 4ml/kg.
- Driving pressures should be 10-15 cmH2O above the PEEP, while keeping the plateau pressure <25 cmH20.
PEEP:
- The PEEP should initially be set at 10 cmH2O, and can be further increased for lung recruitment.
- Patients with right-sided heart dysfunction may further decompensate with high levels of PEEP.
- Patients with left-sided heart dysfunction may benefit hemodynamically from higher levels of PEEP.
FiO2:
- The goal is to minimize the FiO2, ideally < 50%.
- Remember, oxygenation of blood and tissues is determined by the flow and sweep gas settings.
- " After optimizing the sweep and flow, the FiO2 should be adjusted to maintain an arterial O2 saturation of sbout 88-95%.
Respiratory Cycle:
- The respiratory rate is typically set at 10 breaths per minute, and can be adjusted in consort with the sweep gas settings to maintain physiologic pH.
- ELSO guidelines recommend an inverse ratio ventilation strategy (I:E ratio at 2:1).
- At TGH we do not universally employ this strategy, we use it for patients with specific pathology.
- At TGH we generally use a conventional I:E ratio.
Recruitment Manouvers:
- The ELSO guidelines do not recommend performing recruitment maneuvers unless you have determined that the patient's lungs are contributing a significant amount to gas exchange
- To determine if the lungs are contributing, the Cilley test is performed by increasing the FiO2 to 1.0; if the SaO2 rapidly increases to 100% then the test is positive.
- The recommended recruitment maneuvers are.
- Switch to CPAP at 25 cmH2O, or
- PCV at 15/10, rate of 5, I:E at 3:1.
Summary of Ventilation Settings:
Considerations for V-A ECMO:
- Remember in V-A ECMO, some of the patient's still passes through the pulmonary circulation and relies on the lungs for oxygenation.
- This blood is mixed with blood from the ECMO oxygenator in the patient's aorta.
- At relatively low flows, the lungs play a significant role in tissue oxygen delivery.
- Ventilation parameters may have to be adjusted to accommodate for this, and may require deviation from the recommended settings seen in Table 7-1.
Liberation from Mechanical Ventilation:
- Just because a patient is on ECMO, it does NOT mean they need intubation or mechanical ventilation.
- In some cases, patients benefit from being liberated from mechanical ventilation and extubated while on ECMO.
- These are usually patients who are on ECMO as a bridge to recovery.
- Patients on ECMO should have sedation reduced and switched to spontaneous ventilation as early as possible (if it is safe to do so).
- Because native respiration is not required for gas exchange, patients may be extubated on ECMO without passing traditional criteria.
- Extubating patients while on ECMO can help facilitate mobilization and rehabilitation.
Next page: Anticoagulation and ECMO
