Daily Care of the ECMO Patient: Ciruit Settings
While all the routine ICU care still applies to patients on ECMO, there are aspects of their daily care which need to be emphasized.
Any assessment of a patient on ECMO involves reviewing the circuit parameters:
Flow
The flow should never be reduced below 1 litre per minute, as the risk of clot formation becomes very high at low flows
- Flow is not directly controlled by the pump, instead the pump is set to a certain RPM.
- In general, the higher RPM the higher the flow.
- A rule of thumb is that the flow in mL/min is about +/- 500 mL higher than the RPM of the pump.
- For example, if the pump is at 3000 RPM, then the flow through the pump should be anywhere from 2500 to 3500 mL/min.
- If the flow rates are lower than expected for a given pump speed there may be a problem with downstream resistance, or upstream supply.
- Pump speeds above 4500 RPM are associated with high rates of hemolysis.
Consider trying to increase the flow if:
- There are signs of hypoxemia, e.g. decreased SpO2, decreased PaO2.
- There are signs of decreased perfusion of tissue e.g. elevated lactate, decreased urine output (V-A ECMO only).
Consider trying to decrease the flow if:
- The patient is showing recovery of intrinsic ability to oxygenate.
- The patient is showing recovery of cardiac function (V-A ECMO only).
- There is significant hemolysis and the pump speed is above 4500 RPM.
- There is significant chatter and the flow rates are erratic (this may mean your pump speed is too high and it is causing "suckdown" of the return cannula vessel).
Sweep
- The sweep gas rate controls the rate of CO2 removal.
- The FiO2 of the sweep gas helps control the PaO2.
- Sweep gas flow rates vary between 0-15 litres per minute.
Sweep gas adjustments should be considered in the following scenarios:
- The patient develops relative hypercarbia: sweep gas should be increased.
- The patient develops relative hypocarbia: the sweep gas should be decreased.
- The patient develops hypoxemia: the FiO2 of the sweep gas may be increased.
- The patient demonstrates increased work of breathing: the sweep gas may be increased (although this may not work to relieve the work of breathing).
Chatter
- Chatter is the term used to describe periodic erratic movement of the ECMO cannula, sometimes accompanied by a noise.
- Chatter happens when the pump is trying to suck more blood out of the patient than is available.
- The presence of chatter can imply:
- A relative volume deficit, and is often treated by administration of fluids (see troubleshooting section).
- A malposition of the drainage cannula causing intermittent obstruction of flow.
Anticoagulation
In an ECMO circuit, blood is in contact with foreign material, so it has a tendency to clot. A clotted circuit is an immediately life threatening complication and requires emergent surgical intervention.
Although there are differences in anticoagulation strategy, the main principles of management are the same:
- Every patient on ECMO should be anticoagulated unless there is uncontrolled life-threatening bleeding.
- The anticoagulant of choice at TGH is intravenous heparin.
- Adequacy of anticoagulation is measured by the aPTT level.
- The goal UFH depends on several factors, but in general:
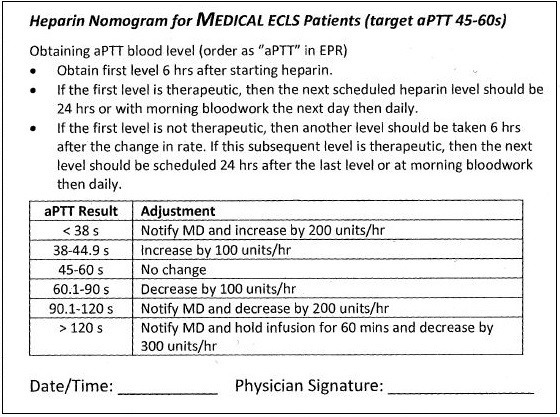
- For "medical" patients, the target aPTT is 45 to 60 seconds.
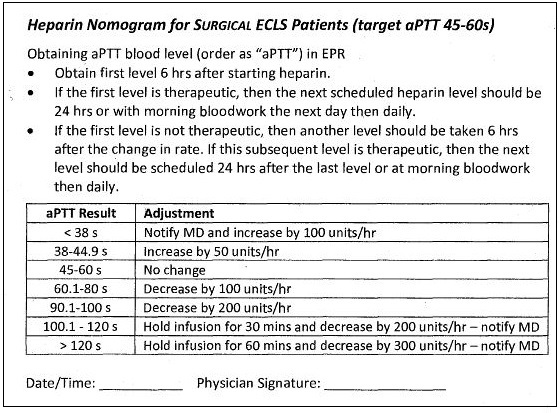
- For patients who have had a recent surgical procedure, the goal is also 45 to 60 seconds, however the parameters are more strict.
- Compare this to someone who is therapeutically anticoagulated for a DVT or PE, where the aPTT target is typically 65-80 seconds.
- Most patients are put on a nomogram with predefined dose adjustments.
- The lower the flow, the higher tendency there is for the patient's blood to clot.
- It is easy to overlook the aPTT level on rounds, but it is of utmost importance.
- The best method of assessing adequacy of anticoagulation is looking for clots on the oxygenator.
Below are the two nomograms we use at TGH for medical and surgical patients. They are almost identical, but the adjustments in surgical patients are smaller and slower.
Next page: Daily care of the ECMO patient: Blood pressure
