ROTEM:
Patients who are anticoagulated on ECLS often have bleeding issues. Because they are on heparin and often critically ill, conventional laboratory measurements (INR, aPTT, platelet count) do not necessarily reflect the patient’s true coagulation status. ROTEM (rotational thromboelastometry) and the PFA-100 assay are tests that are available at TGH which can help get a clearer picture of the patient’s coagulation state.
ROTEM Basics
- It is a test that measures the viscoelastic properties of blood.
- A small sample of the patient’s blood is exposed to a mechanical device which measures the elasticity and strength as the blood is allowed to clot.
- This is converted to an electrical signal which produces a 2D image of the clot formation over time.
- The test is performed by the perfusionists on the second floor next to the operating rooms.
- They require 6 mL of blood to be drawn into a 10 mL syringe and tubed directly to the second floor.
ROTEM Results
- The ROTEM results are reported in the form of a graphic as well as a few numbers. (See images below.)
- The different graphs isolate different portions of the clotting cascade:
- The EXTEM most closely reflects the PT and represents the extrinsic clotting pathway (hence, “EX”-TEM)
- The INTEM most closely reflects the aPTT and represents the intrinsic pathway (hence “IN”-TEM)
- The HEPTEM eliminates any heparin effect on the clot formation, which can expose a coagulopathy which would normally be clouded by the effects of heparin.
- The FIBTEM focuses specifically on fibrinogen function by neutralizing the effect of platelets.
- The APTEM excludes the effects of fibrinolysis, but is otherwise quite similar to EXTEM.
- A rough guide to ROTEM values is as follows:
- Clotting Time (CT): Increased CT reflects a factor deficiency, which usually necessitates administration of FFP.
- Clot Formation Time (CFT) and alpha angle: Increased CFT and alpha angle typically reflects a deficiency in fibrinogen and platelets.
- Maximum clot firmness (MCF): a decreased MCF typically reflects a platelet deficiency, either quantitative or qualitative.
- Maximum clot lysis (ML) and Lysis at 30minutes (LI30): these values represent how much the amplitude has decreased from maximum, and if they are elevated it usually means the patient is hyperfibrinolytic and needs tranexamic acid.
- The visual interpretation of the ROTEM printout helps to guide management as well (adapted from Ony4medical).
- Brandy tumbler: Normal
- Red wine glass: Give FFP
- Test tube: Give platelets
- Champagne flute: Give cryo
- Upside down martini glass: Give tranexamic acid
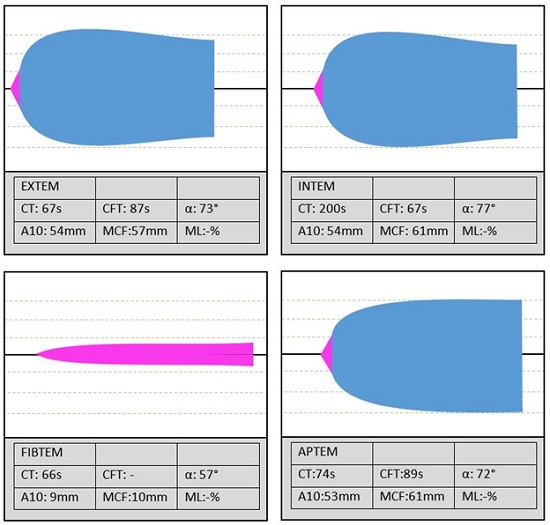
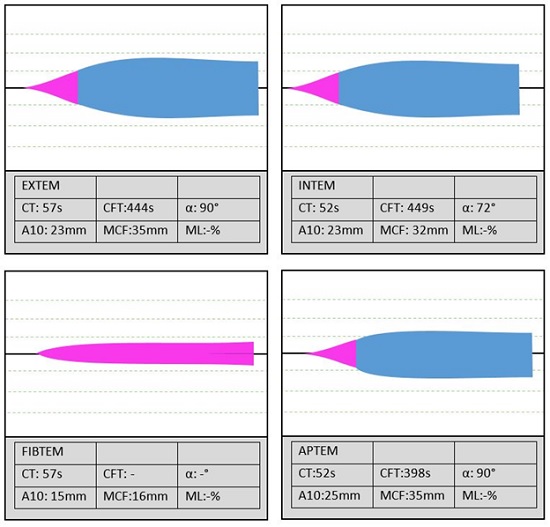
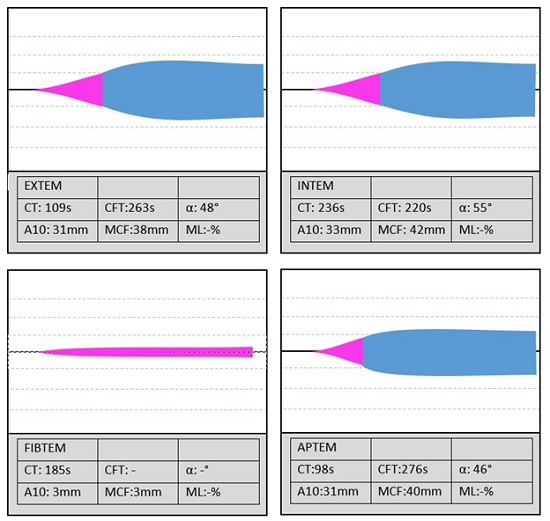
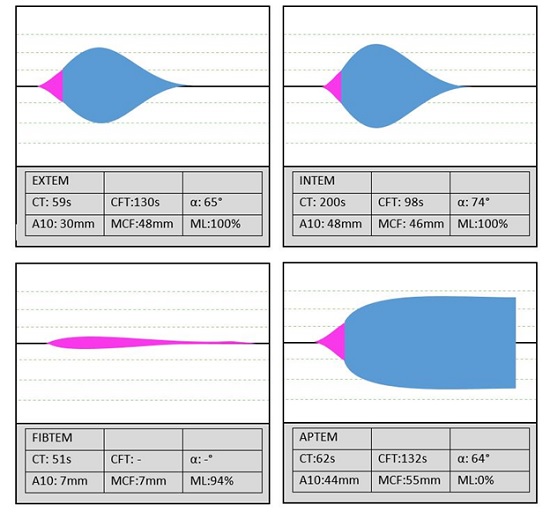
Below are some typical printouts for ROTEM studies (Obtained from http://derangedphysiology.com).
Normal Patient:
Platelet Deficiency(Qualitative or Quantitative):
Low Fibrinogen:
Fibrinolysis:
PFA100
- This test is performed alongside the ROTEM when you send a sample to the lab.
- The details are beyond the scope of this manual, but the result given is the number of functional platelets, and the percentage of the total platelets that these make up.
- This is very handy in patients who have been on cardiopulmonary bypass, or who are on ECLS because they may have very dysfunctional platelets despite having a normal platelet count on CBC.
- For example, if a patient is bleeding and their platelet count is 150,000 on a standard CBC, but their PFA100 shows only a functional platelet count of only 15,000 (10%), then it would be prudent to consider a platelet transfusion despite a “normal” CBC.
