V-A ECMO
V-A ECMO is the ideal configuration for a patient who has refractory cardiogenic shock. Venous blood is drained from a large central vein, typically the inferior or superior vena cava. It is returned to the arterial circulation either centrally (into the ascending aorta) or peripherally (through the femoral artery and into the descending aorta).
In V-A ECMO:
- The ECMO circuit is connected in parallel with the heart and lungs: blood going through the ECMO circuit bypasses the heart and lungs.
- Blood that doesn't go through the ECMO circuit travels through the heart and lungs, and mixes with the ECMO circuit blood in the aorta.
- The pulsatility of the blood flow to the patient's tissues is markedly reduced.
- V-A ECMO is typically used in low cardiac output states refractory to conventional therapies. At TGH the most common reasons for V-A ECMO are:
- Myocardial ischemia
- Dilated cardiomyopathy
- Persistent ventricular tachyarrhythmias
- Myocarditis
- End stage pulmonary arterial hypertension
It is important to understand that V-A ECMO provides hemodynamic support, but it does NOT provide "cardiac support". The jet of blood returning into the aorta generates a huge afterload for the heart to overcome. The presence of V-A ECMO renders the heart vulnerable to overdistension and actually further damage it.
The two main configurations of V-A ECMO are shown below:
Peripheral V-A ECMO
The configuration in the figure below is called "peripheral" V-A ECMO because both the return and drainage cannulas are inserted peripherally via the femoral artery and vein respectively. In peripheral V-A ECMO:
- The distal end of the drainage cannula is in the proximal IVC or right atrium.
- The proximal end of the return cannula is in the abdominal aorta.
- A small second return cannula is placed in the femoral artery just distal to the insertion site of the main cannula to provide blood flow to the ipsilateral lower extremity (this prevents leg ischemia)
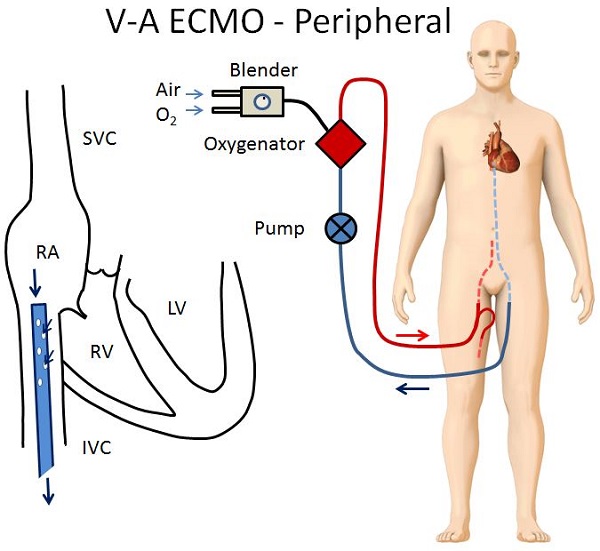
As a result of this configuration, two parallel circulations are created:
- Blood passing through the native heart and lungs that is ejected into the aorta
- The oxygen content of this blood depends on adequate oxygenation and ventilation by the lungs.
- Blood passing through the ECMO circuit that is returned into the abdominal aorta
- Assuming the membrane oxygenator is working properly, this blood will be richly oxygenated.
Blood from these two parallel circulations will mix somewhere in the aorta, and their relative contributions to systemic oxygen delivery is a function of how much flow is going through each circulation. If gas exchange at the patient's lungs are impaired, then deoxygenated blood will mix with the oxygenated blood from the ECMO circuit and tissue hypoxia can occur:
- Territories most vulnerable to hypoxia are those with blood supply from the proximal aorta.
- The coronary arteries supplying the myocardium.
- The innominate artery supplying the right arm and the brain.
- The left common carotid artery supplying the brain.
- In extreme cases, this can present as a "Harlequin" appearance, where the head and upper extremities of the patient appear blue, and the lower half of the patient appears red.
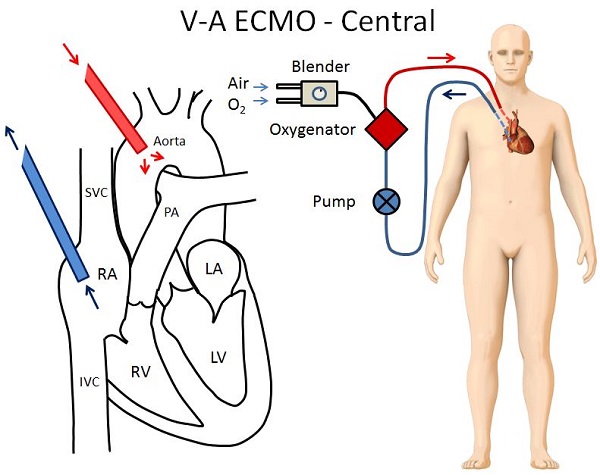
Central V-A ECMO
The configuration in the figure below is called central V-A ECMO because the return cannula is placed directly into the thoracic aorta. In VA-ECMO:
- The distal end of the drainage cannula is in the proximal IVC or right atrium.
- A sternotomy incision is required to place the return cannula directly in the thoracic aorta.
- A larger return cannula can be used compared to central V-A ECMO allowing for greater flows.
- There is no risk of cerebral or coronary hypoxemia.
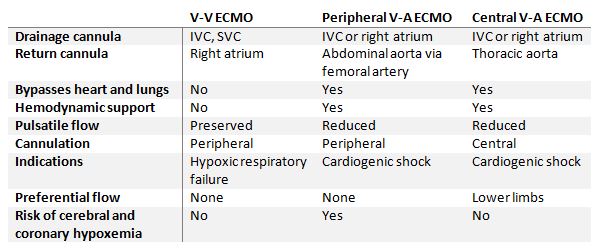
The similarities and differences between V-V and V-A ECMO are summarized in the table below:
Next page: Special ECMO Configurations
